Pain DEFINITION
Pain is defined as suffering or discomfort caused by illness or injury. It is an unpleasant sensory and emotional experience associated with actual or potential tissue damage.
Pain Assessment Questions
- How long have you had this pain?
- What caused the pain?
- What is the current pain level?
- What is the usual pain level?
- What is the pain at its worst?
- What is the pain at its least?
- What are you currently doing to manage this pain?
- Is there anything that you’re doing that’s reducing the pain?
- What pain medications have you taken in the past, and how did they work for you?
- Does the pain move anywhere?
- Describe the pain – is it aching, sharp, deep, shooting?
- Tell me about the worst pain or soreness with movement.
- What makes it hurt more and what helps most?
- When does it hurt most?
- Is it worse when you sit or move?
- Is it worse in the morning or night?
- How long does it last?
- Does it come and go or is it there all the time?
- Does the pain affect sleep, appetite, physical activity, relationships with others, emotions, concentration?
Pain DURATION
Acute Pain
Acute pain generally, refers to pain associated with the acute stage of inflammation, usually for the first 48-72 hours.
Sub Acute
Sub Acute pain after the acute stage but not yet chronic (>72 hrs)
Chronic Pain
Chronic pain refers to pain associated with the stages of healing after the resolution of the inflammatory response. It is commonly used to refer to pain of long duration i.e., more than 3 months
Pain Patterns
Dermal Pain
Dermal pain comes from superficial soft tissues, usually well localized (e.g., a cut in the skin).
Dermatomal Pain
Dermatomes are the areas of skin innervated by a specific nerve root. Deeper structures sharing the same nerve root may express their pain through their corresponding dermatome.
Sclerotomic Pain
A sclerotome is an area of connective tissue or bone innervated by a single nerve root. Sclerotimic pain is pain in any tissue shared by the same nerve root. The pain can either refer pain into the bone or refer bone pain into the more superficial tissues. Sclerotomic pain comes from somatic tissues typically deep, aching & somewhat localized.
Somatic Pain
Somatic pain is generally described as musculoskeletal pain. Somatic pain can be either superficial or deep. Superficial pain arises from nociceptive receptors in the skin. These receptors are also in the mucous membranes, such as in the mouth and nose. A typical pain sensation due to an injury, such as bumping the knee or cutting your lip, results in sudden, sharp pain. Deep somatic pain originates from structures such as joints, bones, tendons, and muscles.
Radicular Pain
Radicular pain comes from nerve roots/ nerve root lesions. It is described as shooting electrical, or burning pain and in a dermatomal pattern. Pain may be felt at the end of a dermatomal area (the most distal point that the sensory nerves associated with that nerve root extends to. Nerve compression distal to the nerve roots may result in a peripheral nerve distribution pattern of pain (e.g., carpal tunnel syndrome).
Visceral Pain
Visceral pain comes from internal organ capsule distension, deep cramping pain that may be sharp at times, often poorly localized in severe cases the pain may be immobilizing (e.g., PMS, intestinal cramps, PMS).
Phantom pain
Phantom pain arises from direct changes in neural pathways & perception of the brain, felt by amputees in the area of the missing limb.
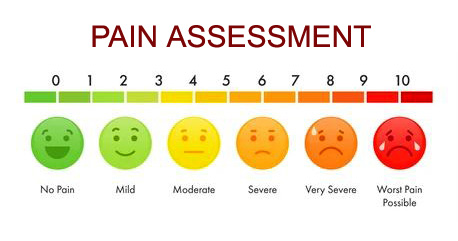
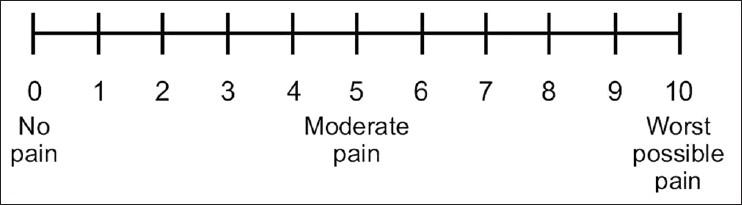
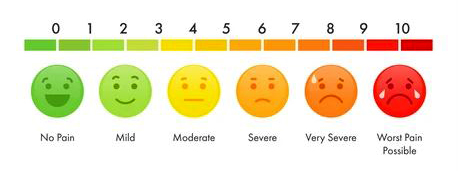
PAIN INTENSITY Measurement
There are 3 main methods used to measure pain intensity. Pain scales have been demonstrated to be both a reliable & valid instrument for measuring the patient’s sense of pain.
1. Visual Analogue Scale (VAS)
In the visual analog scale (VAS), a patient is asked to indicate their perceived pain intensity (most commonly) along a 100 mm horizontal line, and this rating is then measured from the left edge (VAS score).

2. Verbal Rating Scale (VRS)
The VRS pain scale consists of a list of adjectives describing various levels of symptom intensity.

3. Numerical Rating Scale (NRS)
The numeric rating scale (NRS) is a pain measuring tool, commonly used to assess pain severity at that moment in time using a 0 – 10 scale, with 0 meaning “no pain” and 10 meaning “the worst pain imaginable.”
4. Faces Pain Scale
Faces pain scale is a self-report measure of pain intensity recommended for use with younger children & elderly in parallel with numerical self-rating scales (0-10).
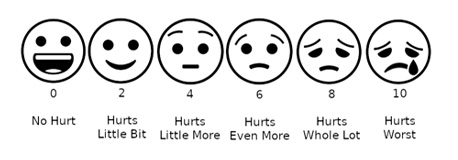
Wong-Baker Faces Pain Scale
Tissue Sensitivity To Pain
Most sensitive tissue to the least sensitive tissue pain:
| Most Sensitive ———> Least Sensitive | |||
|---|---|---|---|
| Skin Fibrous capsule Periosteum |
Tendons Ligaments Subchondral bone |
Cortical bone Muscle Fascia |
Fibrocartilage Articular cartilage Synoviums |