A compartment syndrome is the result of an increase in pressure within the compartments of the lower leg.
- divided by dense, inelastic fascia
- Any of the compartments may be affected, but anterior compartment is more prone ( about 45%)
- Deep posterior compartment syndrome is common as well
The 4 compartments in the Lower Leg:
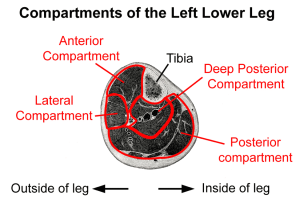
- ANTERIOR COMPARTMENT: contains tibialis anterior , extensor hallucis longus, extensor digitorum,anterior tibial artery, and vein, deep peroneal nerve. (Can be caused by tightness in the gastrocnemius/soleus)
- SUPERFICIAL POSTERIOR COMPARTMENT: gastrocs and soleus
- DEEP POSTERIOR COMPARTMENT: tibialis posterior, flexor digitorum longus, flexor hallucis longus, posterior tibial artery, vein, and nerve, peroneal artery and vein
- LATERAL COMPARTMENT: peroneus longus, brevis
MEDICAL TREATMENT:
- Acute compartment syndrome is treated with an immediate fasciotomy — a surgical procedure where fascia is cut to relieve pressure or tension. Compartment syndrome is a medical emergency that requires prompt diagnosis and treatment to prevent permanent damage to the muscles and nerves. If you suspect compartment syndrome, seek immediate medical attention.
- Chronic compartment syndrome can be treated conservatively with rest and stretching. If this fails, fasciotomy is performed.
Compartment Syndrome Symptoms:
Acute Compartment Syndrome Symptoms (Medical Emergency)
- Bleeding/ swelling within unyielding compartment increases pressure. Pressure may increase to a point where nerve and arteries are compressed. Permanent damage and muscle necrosis may result if fasciotomy is not performed.
- Pain is severe and persistent. Severe pain that doesn’t improve with rest or pain medication and is often out of proportion to the injury.
- Pallor: Pale or shiny skin over the affected area.
- Paralysis: Weakness or difficulty moving the affected limb.
- Paresthesia: Tingling or burning sensations. Sensation may diminish distally.
- Affected compartment hot and harder than unaffected side.
- AF dorsiflexion, extension (toes) and inversion difficult due to pain. Passive stretch of affected compartment is painful.
- Pulselessness: Diminished or absent pulse in the affected area (a late sign).
Chronic Compartment Syndrome
- Symptoms felt with exercise. Pain begins with activity and relieved by rest.
- Increased blood flow into muscle during exercise increases their size and therefore, pressure within the leg compartment.
- Ache and tightness over entire compartment.
- Parasthesia in leg and foot with exercise.
Compartment Syndrome CAUSES:
Causes of Compartment Syndrome:
- BURNS
- Circumferential Burns: Full-thickness burns that encircle a limb can lead to eschar formation, which restricts expansion of the underlying tissues and increases compartment pressure.
- IATROGENIC CAUSES
- Medical Procedures: Certain medical interventions, such as tight bandaging, casts, or prolonged use of tourniquets, can inadvertently increase compartment pressure.
- INFECTIONS
- Severe Infections: Infections causing extensive swelling or abscess formation within a compartment can lead to increased pressure and compartment syndrome.
- INFLAMMATORY CONDITIONS
- Severe inflammation: whether from an autoimmune response or other inflammatory conditions, can cause swelling and increased pressure within a compartment.
- OTHER CAUSES
- Prolonged Immobilization: Remaining in one position for an extended period, especially in a position that restricts blood flow, can lead to compartment syndrome.
- OVERUSE/ OVER TRAINING:
- Chronic Exertional Compartment Syndrome (CECS): Repetitive exercise, especially in athletes, can lead to temporary increases in compartment pressure. This is more common in activities involving repetitive leg movements, such as running or cycling.
- TRAUMA
- Fractures: Broken bones, especially in the arms and legs, can cause swelling and bleeding within the muscle compartment.
- Crush Injuries: Severe trauma, such as being crushed by a heavy object, can lead to significant swelling and increased pressure within a compartment.
- Soft Tissue Injury: Direct trauma to the muscles without fracture can also cause swelling and increased compartmental pressure.
- VASCULAR ISSUES
- Reperfusion Injury: When blood flow is restored to an area that has been deprived of circulation (e.g., after surgery or prolonged tourniquet use), it can cause swelling and increased compartment pressure.
- Bleeding: Internal bleeding from blood vessels within a compartment, often due to injury or surgery, can increase pressure.
- Reperfusion Injury: When blood flow is restored to an area that has been deprived of circulation (e.g., after surgery or prolonged tourniquet use), it can cause swelling and increased compartment pressure.
Compartment Syndrome Massage CONTRAINDICATIONS:
- No Frictions with anti inflammatory medications
- A client with acute compartment syndrome is immediately referred for medical attention.
Massage Therapy Assessment:
- Acute compartment syndrome – refer to a medical doctor
- ROM testing- restricted by pain.
- With anterior compartment syndrome, pain will be on active dorsiflexion and passive plantarflexion
- Length tests — often short antagonists. With anterior compartment syndrome, gastrocs and soleus are short
- Palpation of affected compartment may reveal tightness and defects in the fascia from continued pressure.
- Tibialis posterior Tendinitis ( plantarflex and inversion) — pain will be along the course of the tendon, just posterior to medial malleolus. AR testing for tendonitis is (+)
- Tibial Stress Fracture — pain is sharp and local to fracture site. Pain becomes constant and worse with impact.
- DVT — local tenderness in calf. Homan’s/Ramirez test (+)
Massage Therapy Treatment: (CHRONIC Compartment Syndrome)
- Refer to an MD if acute compartment syndrome – no massage
- Work to compensating structures — low back, gluteals, thighs
- Fascial techniques, passive stretching are used to elongate short, thick fascia. Start with antagonists
- Short gastrocs/ soleus are treated with fascial techniques, interspersed with stretching
- Supine, quads and aductors treatment, especially Trigger points that refer to anterior leg
- Longitudinal fascial techniques to anterior compartment to loosen fascia and reduce pressure. Passive plantarflexion to stretch
- Any adhesions in tibialis anterior treated with cross fiber frictions
- Effleurage and petrissage to entire limb ( toward heart)
SELF CARE:
- Patient rests from activities causing pain
- Proper warm up period may help to reduce rapid bloodflow to compartment
- Self massage to compartment borders
- Stretching the muscles of lower leg starts with antagonists, then progress to affected area
- Patient may need orthotics.