Arthritis Massage: Signs & Symptoms, Massage Procedure, Massage Contraindications
Osteoarthritis (OA) – is a group of chronic, degenerative conditions that the affect joints specifically, the articular cartilage and subchondral bone. Osteoarthritis, commonly called ‘arthritis’ is a gradual condition, known as ‘wear and tear’.
According to arthritis.org, there are more than 100 different forms of arthritis. The most common types include osteoarthritis, rheumatoid arthritis, psoriatic arthritis, fibromyalgia and gout.
Rheumatoid Arthritis (RA) is an autoimmune disease. In RA, the immune system attacks parts of the body, especially the joints. The attack leads to inflammation, which can cause severe joint damage if not treated. This post is about Osteoarthritis Massage .. For Rheumatoid Arthritis Massage >> see Massage for Rheumatoid Arthritis
Psoriatic Arthritis: People with this condition have inflammation of the skin (psoriasis) and joints (arthritis). Psoriasis causes patchy, raised, red, and white areas of inflamed skin with scales.
Fibromyalgia syndrome is a disorder characterized by widespread musculoskeletal pain, affecting muscles and soft tissue. Symptoms of fibromyalgia includes painful trigger/tender points, chronic muscle pain, sleep, memory and mood issues. For Fibromyalgia Massage >> see Massage for Fibromyalgia
Arthritis Signs & Symptoms
- Osteoarthritis occurs almost exclusively in weight-bearing joints (joints in the hands, knees, hips and spine) mostly the knees.
- Joint pain during or after movement
- Tenderness in the joint when light pressure is applied to it
- Stiffness and loss of flexibility. Patient may not be able to move the affected joint through its full range of motion
- Grating sensation. You may hear or feel a grating sensation when you use the joint
- bone spurs. These extra bits of bone, which feel like hard lumps, may form around the affected joint.
- presence of Heberden’s and bouchard’s nodes
- Heberden’s Node – enlargement of the distal interphalangeal
- Bouchard’s Node – enlargement of the proximal interphalangeal
Early stage of Osteo Arthritis: painless
- pain follows joint use, relieved by rest. Pain is local, achy, difficult to pinpoint
- reduced range of motion
- joint stiffness in a muscle until “worked out” – about 30 minutes*
Later stage of Osteo Arthritis:
- 85% of cases are 70+ years old
- Pain sensitive subchondral bone exposed
- Pain at night
- Locally tender
- Crepitus with movement, stiffness and decreased range of motion
- Contracture of muscle crossing joint
- Osteophytes
- Muscle spasms and edema
- Although Osteo Arthritis is non-inflammatory in itself, there my be some inflammation from time to time due to irritation of surrounding structures
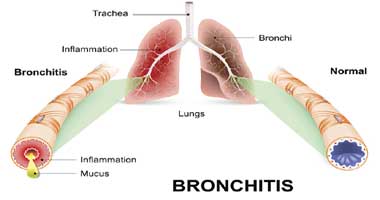
Pathological Process (Normal vs Joint w/ OsteoArthritis)
Normal Joint:
- Synovial joint is composed of hyaline-cartilage covered bone ends
- Connected by fibrous joint capsule
- Reinforced by extra capsular ligaments
- Muscles and tendons cross and control movement
- Joint capsule lined with synovial tissue which produces synovial fluid to nourish and lubricate
- Healthy cartilage is resilient, able to yield to compression, once load is removed, cartilage recovers original shape
- During joint motion, muscles that cross the joint work as shock absorbers and movement controllers – protecting the articular cartilage
Joint with Osteoarthritis:
- Load bearing portions of articular cartilage are affected first
- Collagen fibers break
- Cartilage is avascular, not able to repair itself
- early stage is non-inflammatory
- Cartilage continues to break, becomes thinner and softer
- Vertical clefts develop in cartilage surface
- Cartilage fragments break off into synovial fluid
- These fragments can be caught in between the bones when the joint moves. The joint the locks and is unable to move. This is also known “joint mouse”
- The clefts in the cartilage extend into the subchondral bone
- Loss of cartilage causes the joint space to narrow
- Subchondral bone is exposed = pain
Later stage of Osteo Arthritis massage
- Subchondral bone remodels at areas of friction, thickens
- New bone and cartilage grow at margins of joint to support the joint (this new bone growth is known as bone spurs or osteophytes)
- these osteophytes alter shape, restrict joint movement
- vertebral osteophytes painfully compress nerve roots
- Chronic synovitis – develops when cartilage fragments and enzymes released irritate synovial lining
Causes of Arthritis
- can be idiopathic
- Altered biomechanics
- leg length imbalance, congenital hip dislocation, valgus or varus knees, joint hypermobility, muscle incoordination
- Immobilization – reduces circulation of synovial fluid
- Trauma – acute (fracture) or chronic (occupational overuse, repetitive stress)
- Pathology
Types of Osteoarthritis:
- Primary Osteoarthritis is Idiopathic and may be local (one or two joints) or generalize (three or more joints).
- Secondary Osteoarthritis: is the result of a known cause such as joint trauma, underlying pathology
Arthritis Massage Therapy: CONTRAINDICATIONS
- Avoid heat hydrotherapy if inflammation is present
- Caution when applying overpressure with late-stage Osteo Arthritis due to osteophytes
Arthritis Massage: OBSERVATION/ PALPATION
- Joint enlargement, possible swelling
- Antalgic posture/ Antalgic gait
- hypertonicity in the surrounding muscles
- presence of adhesions, trigger points, tender points
- spasm in muscles crossing affected joint and compensating muscles
- Crepitus, fibrosing of joint capsule, disuse atrophy
- Acute – heat, edema, redness (possible)
Arthritis Massage: ROM & ORTHOPEDIC TESTING
- Active Free ROM is reduced due to pain
- Passive Relaxed ROM is painful, leathery end feel if capsule damaged, bony end feel with osteophytes, muscle spasm and empty end feel if acute
- Active Resisted ROM – weakness and pain
Special Tests: No specific tests to determine OA, but the therapist perform special tests to rule out:
- tendonitis
- bursitis
- facet joint irritation
- nerve root compression
- space occupying lesion
Arthritis MASSAGE TREATMENT PROCEDURE:
- Goals – reduce stiffness, pain, edema, spasm, increase ROM
- Diaphragmatic Breathing
- Work within patient’s pain tolerance
- Hydro – deep moist heat to joint (as long as no secondary inflammation present)
Massage Therapy for Early stage of Osteoarthritis
- Pain free rhythmic mobilization, rocking, shaking
- Proximal to distal treatment
- MFR Myofascial Release Techniques
- Soothing Swedish tech – effleurage, stroking, petrissage to reduce hypertonicity
- Trigger Point treatment with deep muscle stripping and ischemic compressions
- Traction joint
- GTO to muscle crossing joint
- Joint play to affected joint
Massage Therapy for Later stage of Osteoarthritis
- Same as early, may be able to be more vigorous (due to tight muscles)
- Inflammation is a little more common, in later stages due to irritation of surrounding structures. In this case, cool hydro
(OA) Arthritis Self Care
- Appropriate hydrotherapy
- Rest from activity
- Pain free activity
- Pain free stretching/ROM
- Referral to physician, naturopath, physio
- Omega 3 fatty acids